U.S. Surgeon General’s Letter to Prescribers:
What’s Missing From This Puzzle?

Some people find working jigsaw puzzles to be a great way to spend their quiet time. Many of us who have done this recognize the frustration felt when, after finding the right places for the first 499 pieces, the 500th piece turns up missing! That sense of frustration and incompleteness is what I’ve been feeling in the wake of a recent letter from the U.S. Surgeon General to all prescribers in the US.
On August 25th, US Surgeon General, Dr. Vivek Murthy, took the unprecedented step of writing all 2.3 million prescribers in the United States, asking them to sign a pledge to change their ways when prescribing opioid analgesics. Specifically, the letter requests that prescribers: 1) educate themselves about safe and effective pain treatment, citing the CDC Opioid Prescribing Guideline; 2) screen patients for opioid use disorder and see that evidence-based treatment is provided when needed; and 3) talk about, and treat, addiction as a chronic illness, not a moral failing.
We can all agree that more education, better screening, and approaching addiction as a medical condition are good things. Opposing those would be like opposing motherhood and apple pie, and I sincerely hope that every prescriber will take this advice to heart. The challenge is that, while we have here three pieces of a puzzle, there is an important fourth piece that is missing.
Conspicuously absent from this initiative is any mention of pain treatments that are alternatives to opioids. Dr. Murthy’s letter drives home the message that health care providers must stop prescribing so much opioid medication in order to minimize opioid abuse, addiction, and overdose. One can argue about whether or not this will be an effective intervention, but the inescapable fact is that a piece of the puzzle is missing: What are clinicians to do if they don’t prescribe opioids?
Every behavioral health specialist worth his or her salt will say that a cardinal rule is this: Never take something away without giving providing a replacement. The Surgeon General is proposing that we take away opioid prescribing, without carefully specifying that doing so for someone who is benefiting from opioid therapy could be harmful, not helpful. My question for Dr. Murthy is: Why isn’t there anything here about the use of non-opioid treatments for pain? Where is the support for the integrative approach to pain care that the CDC guideline recommends, and that we all know is the only safe and sane way to treat pain?
The Missing Piece Found?
Just as I was despairing and once again throwing up my hands in frustration, another government agency rode to the rescue. On September 1, the National Center for Complementary and Integrative Health (NCCIH) issued a report summarizing current scientific evidence for complementary health approaches for chronic pain. This report suggests that some complementary health approaches can help patients manage some types of chronic pain.
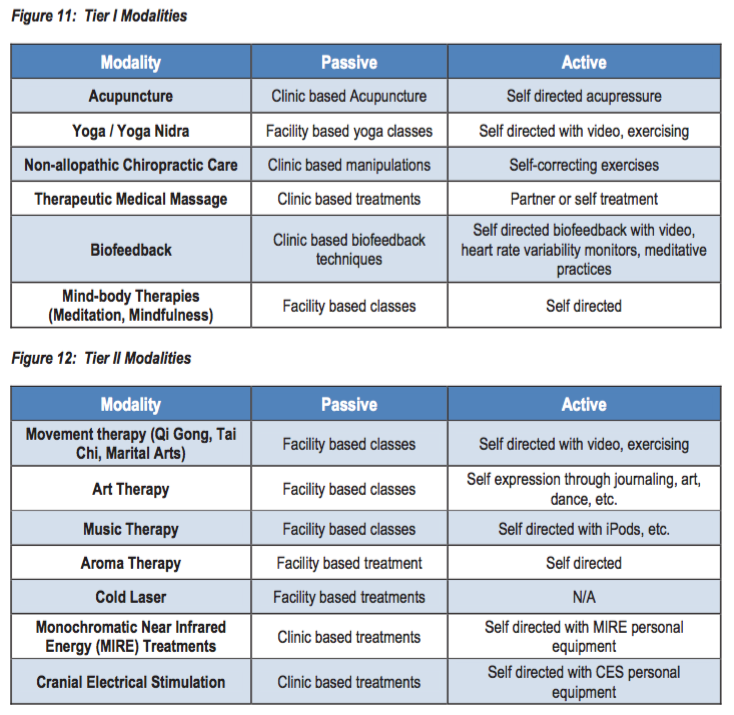
Couple this with a report from the Army Surgeon General’s Pain Management Task Force, which recommends that six key non-pharmacologic treatments (acupuncture, yoga, chiropractic/osteopathic manipulation, massage therapy, biofeedback, and mind-body therapies; see table below) be made available to every current and former service member with chronic pain, and you have some pretty good recommendations. These treatments are the missing piece of the puzzle because they can replace some portion of opioid therapy, minimizing both exposure that could lead to an opioid use disorder and excessive prescribing that leaves behind unused opioids for misuse, abuse, or diversion.
Now we know what the missing piece looks like, but why is it missing? There are a number of reasons, including inadequate education for “traditional” clinicians about these techniques and their uses; a shortage of clinicians providing these treatments, especially in rural and other underserved areas; and reimbursement that is often absent, and frequently inadequate when it is present. For instance, of the six modalities mentioned by the Task Force, Medicare covers only a few types of chiropractic and osteopathic manipulations, and then only for some diagnoses. It covers none of the rest, unless those mind-body therapies are taught in the course of psychotherapy.
Addressing prescription opioid abuse is a complicated and arduous task, requiring multiple approaches. While the government is stepping up, as evidenced by Dr. Murthy’s letter, we need to keep pointing to the missing piece that is support for integrative pain care, and demanding help to find and install that piece. That has been, and continues to be, the primary focus of the Academy’s policy advocacy efforts.
– Bob Twillman, PHD, Executive Director – The Academy of Integrative Pain Management
September 2, 2016
