Managing Compliance
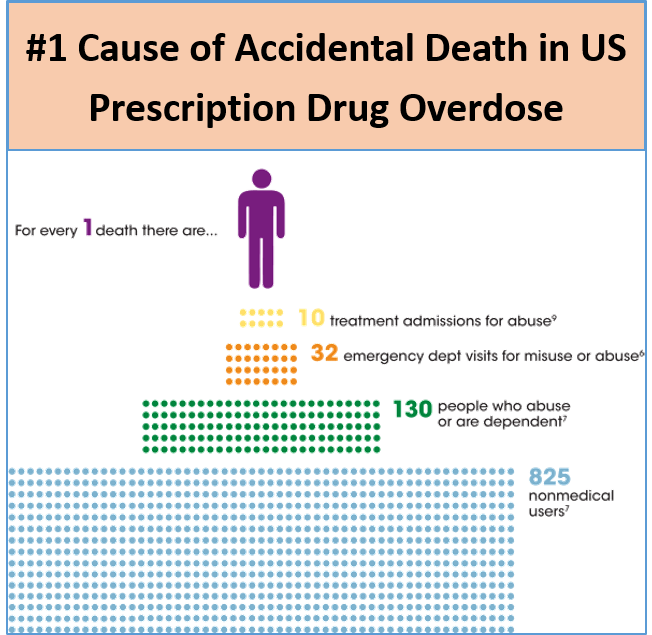
Prescription drug overdose is the number one cause of accidental death in the United States. Beyond these tragic deaths, prescription drug abuse causes many more emergency room visits and billions of dollars in medical expenses. Every incident represents a problem and a potential liability.
Identifying risks early helps manage risks associated with overdose and abuse. Armed with better information in a useful form, physicians can help identify abusers and direct them to treatment earlier in the process.
PastRx does more.
We automatically check every patient. This means you have confidence that every needed check required by your state happens, and that your practice is going above and beyond to assess patient risks.
Our analytics help you see patterns within your patient population as well as anticipating your state or payer’s unsolicited reports. For organizations that self-insure, this insight gives you additional protection through earlier identification of problems.
