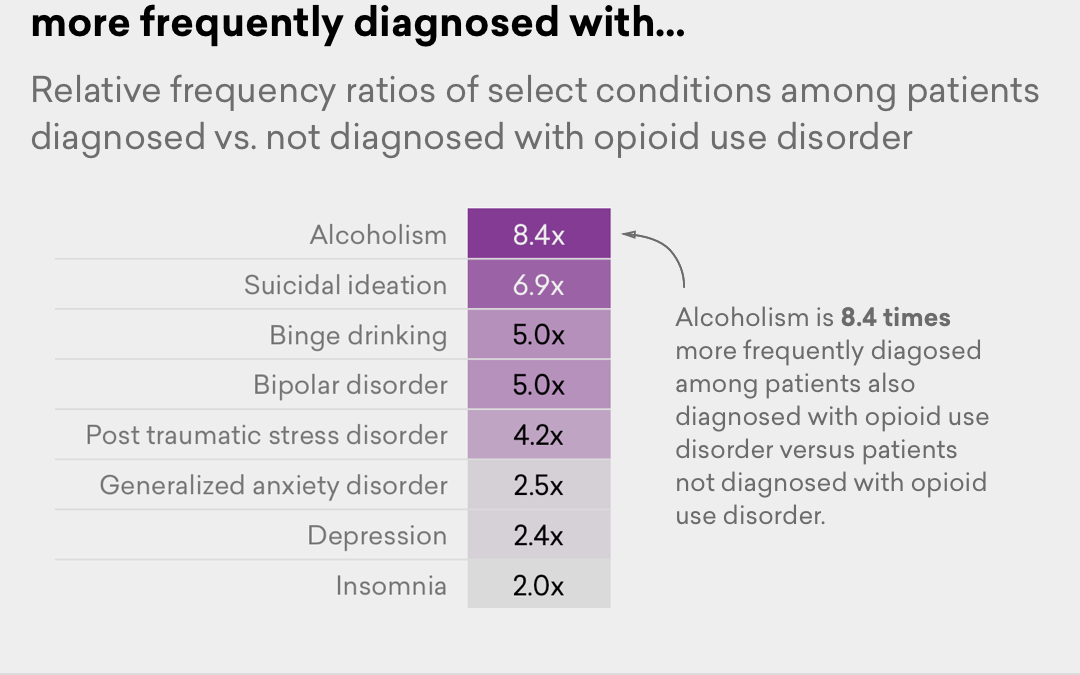
Patients with opioid use disorder are much more likely than the general population to have a host of other health conditions, including hepatitis C, post-traumatic stress disorder, and anxiety.
That’s according to a new analysis from health care company Amino, which culled data from the claims of 3.1 million privately insured patients between 2014 and 2016. It calculated the frequency of a slew of health conditions — from back pain to binge drinking — in patients diagnosed with opioid use disorder. Then, it compared those rates to the general patient population.