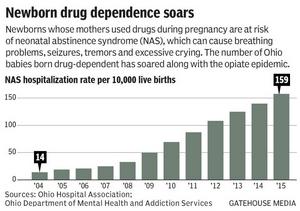
The number of Ohio babies who come into the world sick and craving drugs continues to soar.
That’s more than eight times the rate a decade earlier, in 2005, when there were just 19 such hospitalizations for every 10,000 live births.
“Given the way that the other numbers in the state are going, unfortunately, they were what I expected. I expected the NAS rate to go up,” said Rick Massatti of the Ohio Department of Mental Health and Addiction Services.
Ohio is awash in drug abuse and addiction, at times leading the nation in deaths from heroin and synthetic-opioid overdoses. And women who become pregnant while using drugs can double the harm if they don’t get help quickly.
But awareness and availability of treatment continue to lag.
“As a community, we are failing these moms by not having adequate treatment slots,” said Dr. Barry Halpern, an OhioHealth neonatologist who has helped lead local efforts to care for pregnant drug users and their infants.
– Rita Price
The Columbus Dispatch