Implant for Opioid Addiction Wins FDA Approval
– Probuphine will be implanted under the skin for 6 months to treat addiction
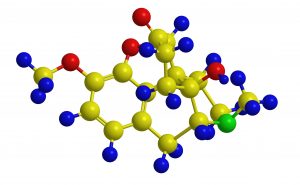
Molecular structure of Oxycodone (Oxycontin) – semisynthetic opioid
The FDA approved an implantable version of buprenorphine (Probuphine) to treat opioid dependence in patients who are already stable on a low dose of the drug, the agency said.
Physicians will have to be trained and certified in how to insert and remove the implant, which is comprised of four rods, each an inch long, that are placed under the skin on the inside of the upper arm for 6 months.
Each implant will contain about 80 mg of buprenorphine, for a total of 320 mg being implanted at once, according to Behshad Sheldon, president and CEO of drugmaker Braeburn Pharmaceuticals. The drug will be released at a constant, low-level dose, the FDA said.
Stable patients include those who have been on 8 mg per day or less of buprenorphine for 3 months or longer without any need for supplemental dosing or adjustments, according to the FDA.
Probuphine will come with a risk evaluation and mitigation strategy (REMS) and a boxed warning about the risk of implant migration, protrusion, expulsion, and nerve damage during insertion and removal.
FDA is also requiring postmarketing studies to establish the safety and feasibility of further treatment with the implant after the initial 6-month period.
Sheldon said the drug will cost less than $1,000 per month. The company will establish a payment assistance program and explore value-based reimbursement programs with insurers, he said.
The company went back to the drawing board and worked with FDA to design a study in a subpopulation of patients who were stable on lower doses of buprenorphine, according to the FDA.
That trial totaled 176 patients who were already taking 8 mg or less daily of buprenorphine — 87 who were treated with Probuphine and placebo sublingual tablets, and 89 who got sublingual buprenorphine/naloxone and a sham implant.
It found that 63% of Probuphine patients had no evidence of illicit opioid use during 6 months of treatment, which was similar to 64% who responded to sublingual buprenorphine — although the FDA’s clinical reviewers voiced concerns about missing data and the company’s definition of a responder during the advisory committee meeting.
FDA acknowledged that the implants “contain a significant amount of drug that can potentially be expelled or removed, resulting in the potential for accidental exposure or intentional misuse and abuse,” and it encouraged doctors to see their Probuphine patients a week after insertion and at least every month thereafter.
Although buprenorphine is currently available as a pill or a sublingual film, the goal of the implant is to improve compliance, the agency said.
The most common side effects included implant-site pain, itching, and redness, and headache, depression, constipation, nausea, vomiting, back pain, toothache, and oropharyngeal pain.
Probuphine will be marketed by Titan Pharmaceuticals and Braeburn Pharmaceuticals.
– Kristina Fiore, Associate Editor – MedPage Today
May 26, 2016
